Antenatal visits in weeks 9 to 13 of gestation roughly make the third month and are almost the end of the first trimester of pregnancy. It plays a pivotal role in the diagnosis and management of certain maternal and fetal conditions.
The patient visits her doctor now for the second time if the pregnancy has been uneventful up until now. The number of visits is decided by how this certain pregnancy is going on. But in the case of a normal, healthy pregnancy, certain guidelines have been provided by higher research authorities.
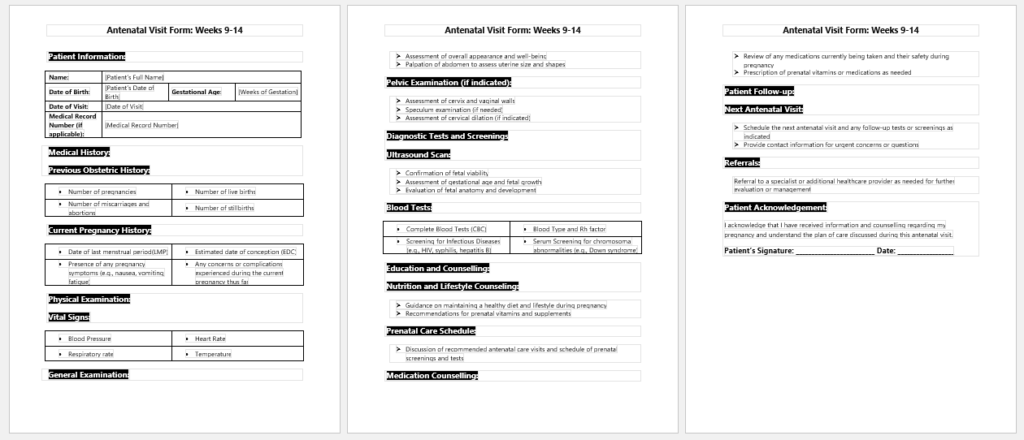
Antenatal visit form
Key components of the visit form are:
Introduction
- It starts with the usual introduction of the patient and the doctor’s name on top, just like her first visit.
- Other details of the patient are not needed here because the previous record from her first visit is sufficient if kept and well maintained.
- Date of examination being held
Weight tracking
The current weight of the patient is measured and compared to the previous weight to keep track of how much she is gaining. In the first trimester, females usually lose some pounds because of morning sickness and being unable to eat properly. But after that, she should, ideally, gain some weight.
Blood pressure and signs of pre-eclampsia
This time carries importance because the physiological changes in the mother start appearing. Usually, blood pressure is measured at every visit, even in a normal, healthy pregnancy. Blood pressure is the first sign of pregnancy-induced hypertension, leading to pre-eclampsia or eclampsia in severe cases. Usually, they don’t appear up to 14 weeks but there is no hard-and-fast rule about it. We should always listen to the patient if she mentions any signs of it. For example
- Raised blood pressure
- Headache along with nausea and vomiting
- Swelling of feet or eyes
- Epigastric pain
- If these signs appear along with raised blood pressure, we need to investigate and be more vigilant about this pregnancy.
Physical examination
- It does include the blood pressure and other vital signs, including the general look and her weight.
- Breast examination is done as part of a
routine examination - A pap smear is taken if necessary
- An abdominal examination can also be done, where we measure the size of the uterus to correlate with her gestational age and ultrasound. This gives us a good idea that the fetus is developing well. However, we cannot measure the uterus size at very early gestation just by an abdominal examination. 12 weeks uterus size and onwards can be measured.
Ultrasounds and investigations
- Abdominal ultrasound now gives us a good idea about the fetus and its surroundings inside the uterus. The placenta starts to develop, and fetal parts are more visible. Fetal nuchal thickness is measured for the diagnosis of Down syndrome. Fetal gestational age is now measured according to crown-rump length.
- Amniocentesis and chorionic villus sampling are done to diagnose some fetal abnormalities, but they are not usually recommended in all pregnancies. It is done only if highly indicated chromosomal defects are to be ruled out. Plus, they are performed at the beginning of the second trimester, ideally.
- Carrier screening of mothers is screened for certain diseases. For example thalassemia, cystic fibrosis, and sickle cell anemia. Usually, diagnosis is already made before pregnancy but if missed, can be done now to avoid any abnormal pregnancies and fetal disabilities later on.
Management plan and counseling
If the mother is diagnosed with any disease that is likely to affect or transfer to her fetus, she is counseled and informed about all the possible consequences of her pregnancy. A time management plan is devised with the full consent of the patient.
Follow up
In the follow-up instructions, she is advised to take proper supplements and proportionate foods. She is advised about her activity, any investigation for the future, and when to come back for her next visit.
- Medical Expense Reimbursement Claim Form
- Patient Enrollment Form Template
- TB Assessment Form for Employment
- Low-Carb Food Shopping List
- Emergency Prep Kit Checklist
- School Immunization Record Sheet
- Home Health Care Log
- New Patient Intake Sheet
- Discontinued Medication Tracker
- Restylane Consent Form
- Dental Assessment Form
- Nutrition Assessment Form
- Clinical Consent Form
- Physiotherapy Consent Form
- Fibromyalgia Journal