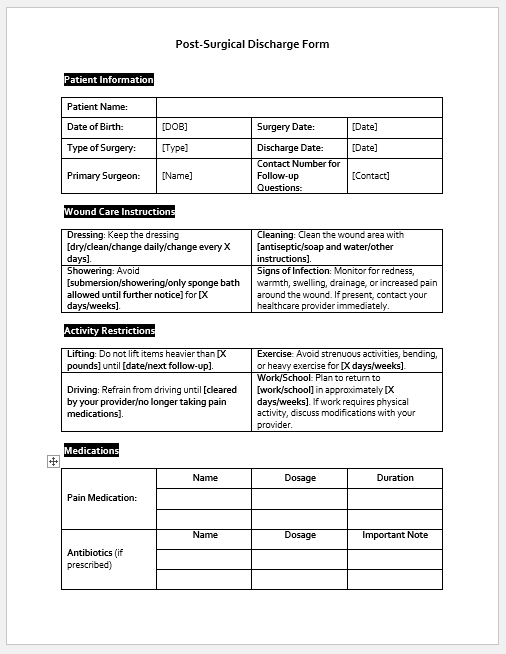
A patient discharge form, sometimes referred to as a patient discharge summary, is a document issued by a hospital to an admitted patient upon discharge.
Who can issue a patient discharge form?
An on-duty doctor or consultant can only decide whether the patient is ready to go home. Only the doctor can issue the form.
Who fills out the discharge form?
A doctor who decides the patient’s discharge and treats the patient during a hospital stay is only authorized to fill out the form and proceed with it to the billing department through the nursing staff.

Word Format (.docx)
Word Format (.docx)
Word Format (.docx)
Word Format (.docx)
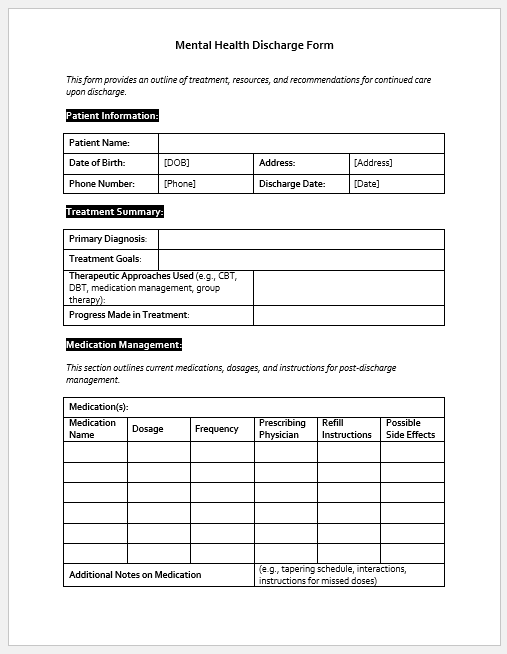
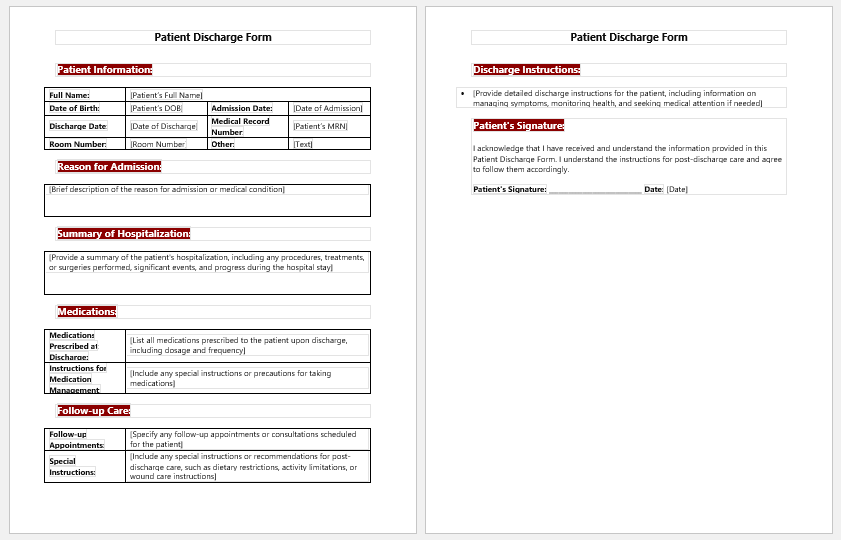
Components of a patient discharge form
A patient discharge form has to include all the basic information about the patient and detailed information about his condition, along with instructions for home. We will discuss them here one by one.
- Patient information: The patient’s name, age, gender, and date of birth, along with their medical record number, if issued by the hospital, must be filled in very carefully. This is serious; we do not want to mix patients with the same names. The patient’s contact number and email address, if any, are also very important to mention.
- Reason for Admission: The patient’s complaints about the patients for whom he was admitted to the hospital must be presented, and all the details about his complaints must be mentioned in the discharge form. That is why the patient’s history is always emphasized.
- Diagnosis at the time of admission: The diagnosis is necessary to fill out the form. Based on the presented complaints, a doctor diagnoses the patient, which is the only justification for admission to the hospital.
- Treatment provided at the hospital: In the patient discharge form, the doctor has to write how he was treated based on his history, examination, and diagnosis. He has to mention all the drugs, whether oral, intravenous or through any other route of administration, with details. If any investigations were done, they are mentioned in their final reports. If a patient is treated by surgery, the procedure and per-operative findings are to be written in the treatment column at the hospital.
- Condition on Discharge: As medical professionals, we must take every step carefully and document it even more carefully. The condition on discharge is a huge responsibility for the hospital and must be assessed and filled out accordingly.
- Important Dates: Important dates like the date and time of admission, the date of discharge, and the duration of stay at the hospital should be written down.
- Medication on discharge: Even if discharged from the hospital, a patient is sometimes prescribed oral medicine at home. This occurs almost always in the case of surgical patients. So, it is the prime duty of the doctor to fill out this portion of the discharge summary with the proper name of the drug, the appropriate dosage, the frequency, and for how long the patient has to take this medicine.
- Instructions on Discharge: In the end, the patient is given some instructions on diet, activity, wound care, and following up on a plan for when he has to return for a checkup.
- Nursing Documentation Templates
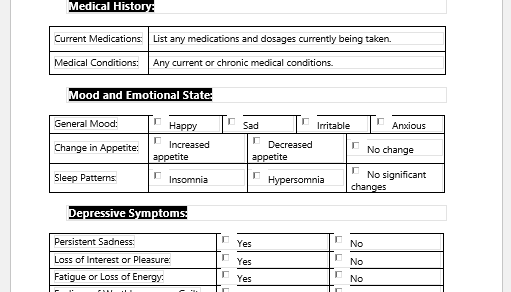
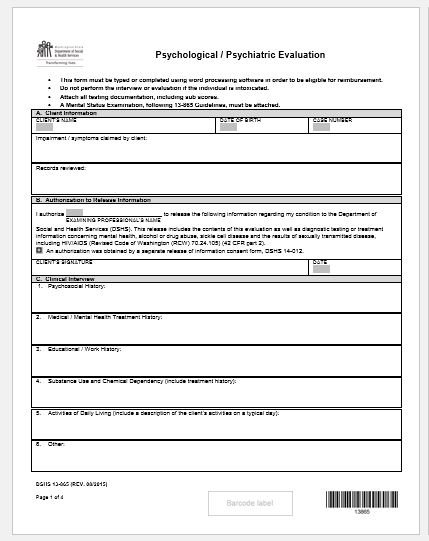
- Mental Health Evaluation Forms
- Forms Used by Pediatricians
- Various Forms Related to Pregnancy Verification
- Common Forms Used by ENT Specialists
- Pain Diary Worksheet Template
- Forms Commonly Used by Old Age Homes
- Medical Treatment Consent Form
- Home Exercise Program Worksheet
- Forms Used for Mental Health Assessment
- Forms Used by Psychologists
- Medical Forms Commonly Used by/for Students
- Assessment Consent Form
- Forms Used by an Anesthesiologist
- Not Fit to Fly Certificate Template