When a patient is admitted to the hospital, concerned doctors and paramedical staff must keep examining the patient to know his current status. We want to know the health status of the patient, and ideally, he is examined every shift.
What kind of examination is required depends on where he is admitted and for what reasons. All the relevant systemic and general physical examinations are done every 8 to 10 hours. If anything noticeable is identified, it is reported and treated immediately. So, the purpose of the examination is to provide effective treatment and prompt patient care.
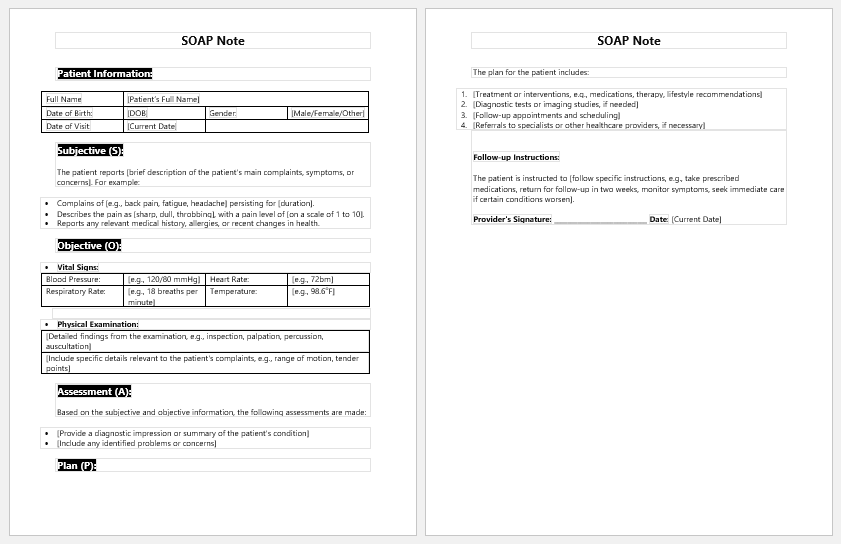
What is SOAP???
Soap is an acronym that is used while examining the patient, especially in the inpatient department. It includes;
- Subject
- Objective
- Assessment
- Plan
We will discuss them one by one.
Subjective
In the examination of the patient, the presenting complaints are mentioned in the subjective portion of the soap note. For example, if a patient in surgery is examined on the next day of surgery, he may complain of indigestion, constipation, excessive pain, nausea, etc. So, all such complaints are mentioned in the subjective portion.
Objective
A general and specific examination done by the doctor is written in the objective. We can write vitals and systemic examinations, and if any significant finding is observed, we mention it in the objective.
Assessment
In the assessment, we document the overall condition of the patient or the diagnosis of the patient. For example, gastroenteritis, hyperemesis, etc. are listed under the heading of assessment.
Plan
The final strategy and management plan are written under the heading of the plan.
SOAP form with body
This specific soap for the body is for the muscular examination of the patient.
- The name of the patient and date are written on the top of the form, as is the name of the company where the examination is being held.
- Then there is a long list of names of muscles that have to be examined under the protocol of SOAP, as discussed in the above lines.
- Starting from the skull muscles, the normal function and tone of the skull muscles are checked, for example, the occipitofrontalis, which is examined by asking the patient to frown and make horizontal wrinkles on the forehead.
- Then there is a group of muscles that join the upper body with the trunk and are called the muscles of the shoulder girdle. These muscles are checked by telling the patient to perform certain functions.
- Muscles of the trunk and abdomen are also tested by their specific tests.
- Muscles of the thigh, like the tensor fascia late, the rectus femoris, and the gluteus muscles of the hip, are tested by performing the normal functions at specific joints.
- Similarly, the muscles of the upper and lower limbs are tested.
- The entire muscle group is tested for tone and function, and their power is checked at every level.
- This soap form is specifically for neurological examination if the patient has come and complained about weakness or numbness at any level.
- Diabetes Travel Letter
- Persmission Letter for Eatables in Office due to Diabetes
- Diabetes Letter to Employer
- Trackers for Medical Facilities
- Nursing Documentation Templates
- Letters for being Unfit to Travel
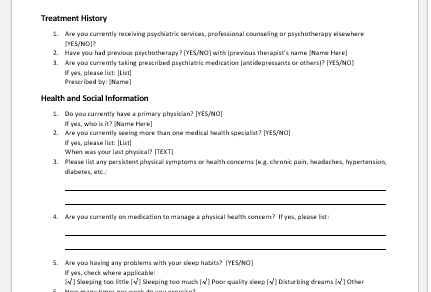
- Mental Health Evaluation Forms
- Forms Used by Pediatricians
- Various Forms Related to Pregnancy Verification
- Common Forms Used by ENT Specialists
- Patient Registration Confirmation Messages
- Quotation Letter for Medical Services
- Mental Health Letter by Doctor
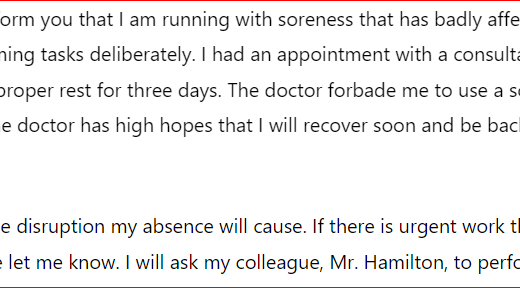
- Excuse Letter for Absence due to Medical Checkup
- Response Letter to Feedback on Improvement in Hospital