Pain is an unpleasant sensation that indicates something is wrong somewhere in the body. However repulsive it may seem, it is sometimes a lifesaver. It is a natural way to urge a person to seek medical advice.
Types of Pain
Pain can be classified into two types: acute and chronic. Acute pain occurs suddenly and usually follows an injury. It may be treated by managing the underlying injury. However, chronic pain persists for weeks, months, or years and is associated with chronic illnesses. Another type of pain is acute-on-chronic pain when a new pain stimulus is superimposed on previous pain caused by chronic disease.
Pain can occur in any body part, and everybody has experienced it. The nature of pain can describe the cause of pain. Pain is pricking, aching, sharp, dull, throbbing, stabbing, pinching, tingling, or burning in nature.
Pain may be classified as:
- Nociceptive: This is the normal response to obnoxious stimuli. It may be somatic (muscular, joint, or cutaneous pain) or visceral (pain involving organs).
- Neuropathic pain: It originates from any abnormality in the nervous system, such as diabetic neuropathy.
- Inflammatory pain is the type of pain that occurs in response to inflammation caused by injury or infection.

Grading Pain Intensity
Pain is graded according to intensity into mild, moderate, and severe forms. Pain severity is classified by the Stanford Pain Scale, where 0 describes no pain and 10 shows that the patient cannot move. 1 is for minimal pain, 2 is for mild pain, 3 is for discomfort, and 4 is for moderate pain. When the patient is distracted because of his pain, it is described by a score of 5; 6 is for distressing pain, which makes the patient give up his work. When the pain is unmanageable, the score is 7, 8 for intense, and 9 for severe pain, which means that all the patient can think of is his pain.
Patient Pain Assessment Form
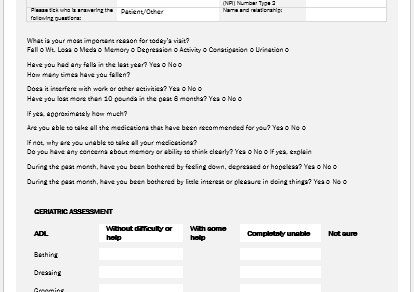
There are various methods to quantify pain. They help in treating the pathology behind them. A mild painkiller might not be helpful in excruciating pain. On the contrary, mild pain does not require narcotic analgesics. The essentials of the patient pain assessment form are:
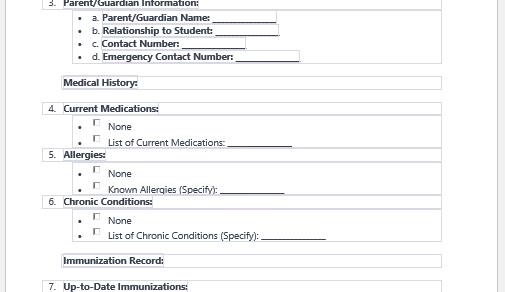
- The patient’s information includes name, age, sex, father’s name, address, contact number, and email address.
- History of current and past medical conditions, drugs, allergies, surgeries, family history, and clinical examination findings.
- A referring physician with credentials.
- Pain scale.
- Description of pain in terms of onset, severity, radiation, patterns, duration, site, associated, relieving, and aggravating factors.
- The tolerance level of pain, worst pain, best pain, effects of pain, limitations, and disabilities.
- Patient’s goal for pain control.
- Privacy and confidentiality agreement.
- Full name and signature of the patient. Date, location, and time of filling out the form.
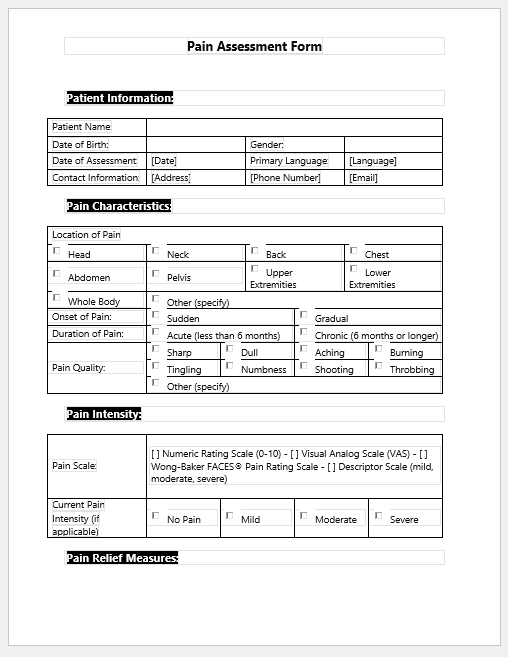
Pain Assessment Form Size: 72 KB
- Diabetes Travel Letter
- Persmission Letter for Eatables in Office due to Diabetes
- Diabetes Letter to Employer
- Trackers for Medical Facilities
- Nursing Documentation Templates
- Letters for being Unfit to Travel
- Mental Health Evaluation Forms
- Forms Used by Pediatricians
- Various Forms Related to Pregnancy Verification
- Common Forms Used by ENT Specialists
- Patient Registration Confirmation Messages
- Quotation Letter for Medical Services
- Mental Health Letter by Doctor
- Excuse Letter for Absence due to Medical Checkup
- Response Letter to Feedback on Improvement in Hospital
- Letter to a Mother Who Miscarried
- Patient Feedback Letter Complaining on Issues or Incidents
- Letter to Family about Miscarriage